|
||||||||||||||
|
||||||||||||||
Menopause marks a significant transition in a woman’s life, bringing hormonal shifts that can increase the risk of several health conditions. As estrogen levels decline, various physiological changes take place, making postmenopausal women more susceptible to cardiovascular disease, osteoporosis, metabolic disorders, and cognitive decline. Understanding these risks and undergoing appropriate screenings can help in early intervention and preventive care.
 |
1. CARDIOVASCULAR DISEASE (CVD)
One of the most concerning risks associated with menopause is heart disease. Estrogen plays a protective role in maintaining healthy blood vessels and cholesterol levels. Its decline leads to increased LDL, reduced HDL, higher blood pressure, and arterial stiffness, all of which contribute to cardiovascular disease.
The risk of heart disease increases substantially for women during and after menopause. Although exact prevalence rates vary, research indicates that nearly 45% of women aged 20 and older are affected by some form of cardiovascular disease. The menopausal transition is marked by significant hormonal shifts, particularly a decline in estrogen, which reduces its cardioprotective effects and heightens the risk of cardiovascular complications. Notably, women who undergo natural menopause at a later age tend to have a lower risk of cardiovascular disease and mortality. Given these factors, it is essential for women experiencing menopause to actively monitor their heart health and adopt preventive strategies.
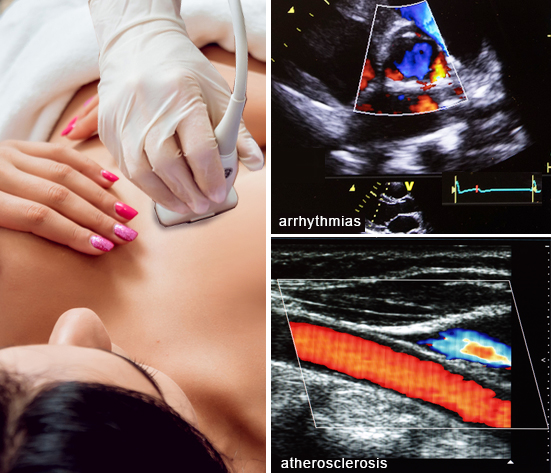
IMAGING HEART HEALTH Carotid ultrasound is also crucial for detecting early atherosclerosis, a key driver of heart disease. By evaluating plaque buildup and arterial thickness, it identifies cardiovascular risks before major events occur. Since heart disease risk rises postmenopause, early vascular screening allows for timely preventive strategies.
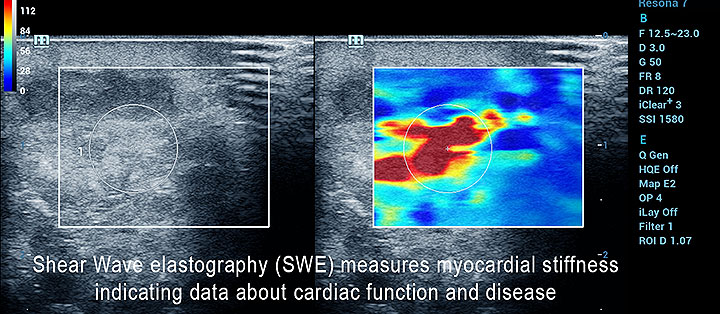
Spasticity: Ultrasound elastography (USE), particularly shear wave elastography (SWE), shows promise as a non-invasive tool for assessing spasticity and monitoring treatment efficacy. While further research is needed to establish its reliability and validity, elastography is a well-established ultrasound imaging technique that measures tissue stiffness or elasticity. It has been widely used for liver fibrosis assessment and is now being explored off-label for other organs. In the context of spasticity, SWE can quantify muscle stiffness, potentially offering a more objective measure than traditional clinical assessments. Incorporating ultrasound into routine assessments enables early intervention, guiding lifestyle and medical management to reduce heart disease risks. Given that cardiovascular disease is the leading cause of death in women, proactive imaging supports a healthier transition into menopause. |
Types of checkups available:
Lipid Panel: Monitors cholesterol and triglyceride levels.
Blood Pressure Monitoring: High blood pressure is a silent risk factor for heart disease.
Blood Glucose and Hemoglobin A1c: Helps detect diabetes or prediabetes, which increases heart risk.
Electrocardiogram (ECG) or Stress Test: Assesses heart rhythm and function, especially for those with symptoms or risk factors.
 |
2. OSTEOPOROSIS AND BONE HEALTH
Estrogen is crucial for bone density maintenance. Its decline accelerates bone loss, increasing the risk of osteoporosis and fractures, particularly in the hips, spine, and wrists.
Types of checkups available: Bone Density Scan (DEXA Scan): Measures bone mineral density and assesses fracture risk. Vitamin D and Calcium Levels: Ensures adequate levels for bone strength. Parathyroid Hormone (PTH) and Thyroid Function Tests: These help assess calcium metabolism and overall bone health.
 |
3. BREAST AND REPRODUCTIVE HEALTH
The risk of breast cancer and other gynecological conditions increases with age, making routine screenings crucial.
Types of checkups available: Mammogram: Detects early signs of breast cancer. Pap Smear and HPV Test: Screens for cervical cancer. Pelvic Ultrasound: Assesses the uterus and ovaries for abnormalities.
PROACTIVE SCREENING • Bone Density Test: Request a bone density scan if you have not had one by menopause or age 50. |
 |
4) STUDYING MENOPAUSE-RELATED HAIR LOSS
MENOPAUSE adds a layer of complexity as she breaks down triggers from hormonal imbalance, physiological stressors and the link to one's personal health. The SCALPSCAN protocol applies advanced ultrasound interpretation to detect (and even possibly predict) the pathological line that leads to alopecia. This can lead to scarring (cicatricial)- where hair follicles are destroyed leading to temporary hair loss that can potentially regrow.
 |
5) COGNITIVE DECLINE AND BRAIN HEALTH
Studies suggest that estrogen has neuroprotective properties, and its decline may contribute to an increased risk of cognitive decline and conditions like Alzheimer’s disease.
Types of checkups available: Cognitive Screening (e.g., MoCA or MMSE): Helps detect early signs of cognitive impairment. Vitamin B12 and Folate Levels: Essential for brain function and mental clarity. Neurological Assessment: For those experiencing memory loss or cognitive difficulties.
 |
6) METABOLIC SYNDROME AND WEIGHT GAIN
Menopausal women often experience weight gain due to hormonal changes and a slower metabolism. This increases the risk of metabolic syndrome, a cluster of conditions that heightens the risk for heart disease, stroke, and diabetes.
Types of checkups available: Body Mass Index (BMI) and Waist Circumference Measurement: Evaluates obesity-related risk factors. Fasting Blood Sugar and Insulin Levels: Screens for insulin resistance and diabetes. Liver Function Tests: Helps detect fatty liver disease, often linked with metabolic syndrome.
 |
7) Hormonal and Thyroid Function
Hormonal imbalances, including thyroid dysfunction, are common in menopausal women and can mimic menopause symptoms such as fatigue, weight gain, and mood swings.
Types of checkups available: Thyroid Panel (TSH, Free T3, Free T4): Screens for thyroid dysfunction. Sex Hormone Levels (Estrogen, Progesterone, and Testosterone): Helps assess hormonal imbalances.
Conclusion
Menopause brings significant changes that can impact long-term health, but proactive checkups and lifestyle modifications can help mitigate these risks. Women should work closely with their healthcare providers to create a personalized health monitoring plan. Early detection and preventive care are key to maintaining optimal health and well-being during and after menopause.
Menopause is a natural phase of life, but its symptoms can be challenging. Conventional medicine offers
several well‐researched solutions to help manage symptoms effectively. Whether you're experiencing hot
flashes, mood swings, or bone density loss, there are proven medical treatments available to support your
well‐being.
Hormone Therapy (HT)
|
Non‐Hormonal Prescription Medications
For those who cannot or choose not to take hormone therapy, several non‐hormonal options are available:
• SSRIs & SNRIs – Selective serotonin reuptake inhibitors (SSRIs) and serotonin‐norepinephrine reuptake
inhibitors (SNRIs), such as paroxetine and venlafaxine, can help reduce hot flashes and improve mood
stability.
• Gabapentin – Originally designed for seizures, this medication has been found to relieve hot flashes,
especially for those who experience them at night.
• Clonidine – A blood pressure medication that may help some women with hot flash management.
• Ospemifene – A selective estrogen receptor modulator (SERM) that can improve vaginal dryness and
discomfort during intercourse.
Vaginal Estrogen Therapy
For those experiencing vaginal dryness, irritation, or painful intercourse, localized estrogen treatments such
as creams, rings, and tablets offer targeted relief with minimal systemic absorption. These options help
restore vaginal tissue health and comfort.
Osteoporosis Prevention and Bone Health
Menopause‐related hormonal shifts can lead to bone density loss, increasing the risk of fractures.
Prescription medications such as bisphosphonates (e.g., alendronate, risedronate) and denosumab help
maintain bone strength and prevent osteoporosis‐related fractures.
Personalized Medical Guidance
Navigating menopause treatments can be overwhelming. A healthcare provider can help assess your
symptoms, health history, and personal preferences to develop a tailored plan that balances benefits and
potential risks.
While conventional treatments provide effective symptom relief, many women choose to integrate alternative therapies and lifestyle changes for a more holistic approach to menopause management. Explore our additional resources to find the best combination for your journey.
Explore More:
• Conventional Solutions – Learn about medical treatments and HRT.
• Alternative Care – Discover holistic and functional health approaches.
• Lifestyle Changes – Nutrition, exercise, and stress management tips.
 |
The Role of Diet in Menopause
Nutrition plays a crucial role in managing menopause symptoms. A balanced diet rich in whole foods, healthy
fats, and plant‐based proteins can help stabilize hormones and improve energy levels. Incorporating foods
high in phytoestrogens—such as flaxseeds, soy, and legumes—may alleviate symptoms, while reducing
processed sugars and caffeine can help prevent energy crashes and mood swings. MENONEXT offers meal
planning guides and expert advice to help you make informed dietary choices. (See our complete section about LIFESTYLE CHANGES)